The study, led by scientists from the Pasteur Institute, CNRS, Inserm, University of Paris and Assistance publique-Hôpitaux de Paris, was published on 3 May in the journal Science Translational Medicine.
Discover our latest podcast
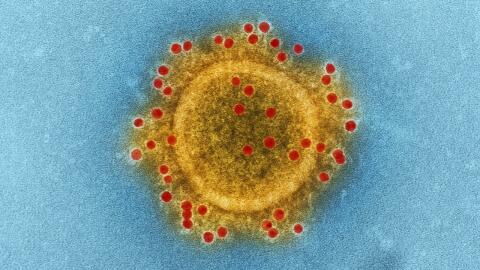
[The virus] infects sensory neurons and causes persistent inflammation of the epithelium (tissue of cells covering the external or internal surfaces of the body, editor's note) and the olfactory nervous system.
One of the hypotheses accepted until now was that 'transient oedema in the olfactory slits prevented the passage of air that carries odorous molecules to the olfactory nerve cells—' the sensation of a blocked nose experienced during a cold. However, Inserm states that
This study unexpectedly shows that the classic RT-qPCR tests performed on nasopharyngeal swabs can prove negative even though the virus persists at the bottom of the nasal cavities, in the olfactory epithelium.
In laymen's terms, a nasal swab can reveal an infection when a PCR test comes back negative.
A gateway to the brain
The research identified several stages in the loss of smell, the first being 'the disappearance of the cilia carried by the sensory neurons,' which 'allows the reception of odorant molecules by the sensory neurons.' The loss of smell is also the consequence of 'a degradation of the sensory organ located at the bottom of the nasal cavities:' the sensory neurons can be infected, as well as the olfactory nerve and the olfactory nerve centres of the brain, says Inserm.
Work carried out on hamsters has highlighted the fact that 'the virus, once it has entered the olfactory bulb, spreads to other nervous structures where it induces a significant inflammatory response', explains Hervé Bourhy, from Inserm, co-author of the study. It is the infection of olfactory neurons that could explain why SARS-CoV-2 can cause psychological or neurological reactions—these hypotheses need to be studied further. As for the durability of the anosmia, it can be attributed 'to the persistence of the virus and inflammation in the olfactory mucosa.'
Rehabilitating your nose
The process is not irreversible in the majority of cases. A document from the HAS indicates that 'the duration of the recovery process will depend on the neurosensory damage and may range from a few months to two years on average,' depending on the types of virus already known. The HAS specifies that in the event of persistence 15 days after the onset of symptoms, the doctor may propose that the patient wash his or her nose with physiological serum, 'associated with olfactory rehabilitation,' which must be started 'as soon as possible.' This is currently the only treatment that has proven its effectiveness.
Olfactory re-education consists of stimulating the olfactory memory and the nostrils by smelling various characteristic scents (vanilla, coffee, essential oils, etc.) twice a day, combined with a written follow-up.